Diet-Related Colic: When to Suspect It and What to Do
Please note that the following should be seen as general information about colic in relation to diet. For specific advice, ...
Read MoreImportant notice to customers — product packaging changesLearn More
NEW FOOD PACKAGING IN STORE NOW
From August 2018, customers will notice our rebranded food packaging start to appear on shelf in all major stockists.
 CURRENT Packaging
CURRENT Packaging

 new Packaging
new Packaging
We are excited to announce our new packaging will start to appear on shelf from August 2018. This transition to new packaging will occur over a number of months. During this time there will be a mix of current and new packaging on shelf.
There are no major changes to these products, in some instances there is a small name change or slight recipe improvement, see below for the full details.
Products purchased via the website will be delivered to customers in our old packaging until the end of October. From November, products ordered from the website will be delivered in the new packaging.
Please note, our Infant Formula packaging will not be rebranded until later in 2019.
For any questions, connect with our team of accredited practising Dietitians on +61 3 6332 9200
Product name changes
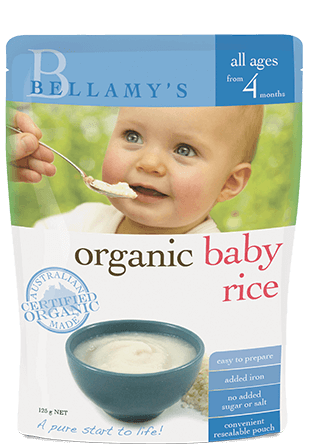 CURRENT Packaging
Organic Baby Rice
CURRENT Packaging
Organic Baby Rice

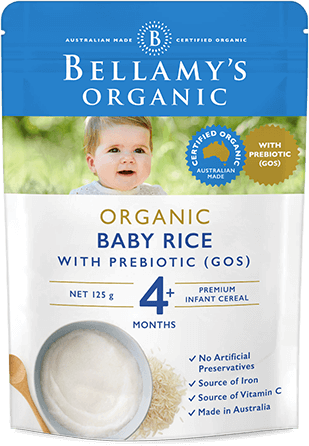 NEW Packaging
Organic Rice with Prebiotic (GOS)
Note: Our Baby Rice recipe has been upgraded to now include GOS Prebiotic
NEW Packaging
Organic Rice with Prebiotic (GOS)
Note: Our Baby Rice recipe has been upgraded to now include GOS Prebiotic
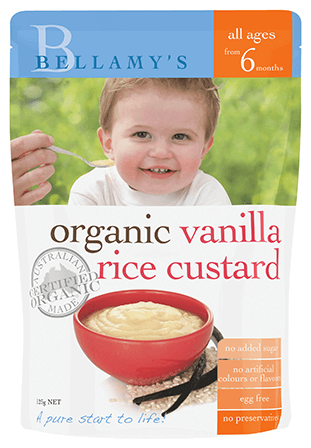 CURRENT Packaging
Organic Vanilla Rice Custard
CURRENT Packaging
Organic Vanilla Rice Custard

 NEW Packaging
Organic Milk & Vanilla Baby Rice
NEW Packaging
Organic Milk & Vanilla Baby Rice
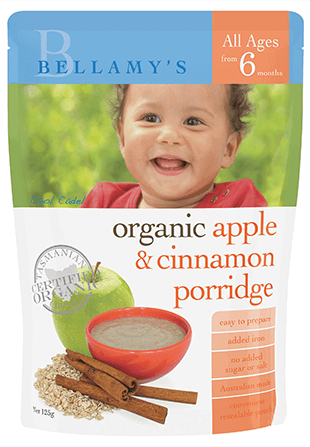 CURRENT Packaging
Organic Apple & Cinnamon Porridge
CURRENT Packaging
Organic Apple & Cinnamon Porridge

 NEW Packaging
Organic Apple & Cinnamon Baby Porridge
NEW Packaging
Organic Apple & Cinnamon Baby Porridge
 CURRENT Packaging
Organic Banana, Pear & Mango
CURRENT Packaging
Organic Banana, Pear & Mango

 New Packaging
Organic Banana, Pear, Apple & Mango
New Packaging
Organic Banana, Pear, Apple & Mango
 CURRENT Packaging
Organic Mango, Blueberry & Apple
CURRENT Packaging
Organic Mango, Blueberry & Apple

 New Packaging
Organic Blueberry, Mango & Apple
New Packaging
Organic Blueberry, Mango & Apple
 CURRENT Packaging
Organic Peach & Apple
CURRENT Packaging
Organic Peach & Apple

 New Packaging
Organic Grape, Apple & Peach
New Packaging
Organic Grape, Apple & Peach
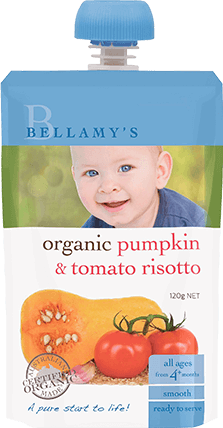 CURRENT Packaging
Organic Pumpkin & Tomato Risotto
CURRENT Packaging
Organic Pumpkin & Tomato Risotto

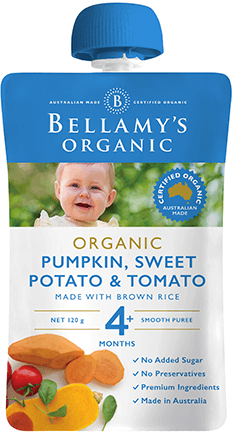 New Packaging
Organic Pumpkin, Sweet Potato & Tomato
New Packaging
Organic Pumpkin, Sweet Potato & Tomato
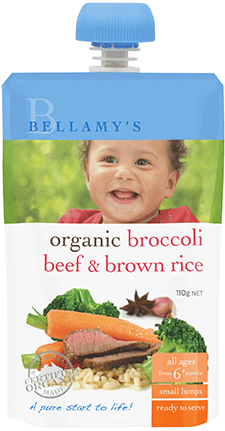 CURRENT Packaging
Organic Broccoli, Beef & Brown Rice
CURRENT Packaging
Organic Broccoli, Beef & Brown Rice

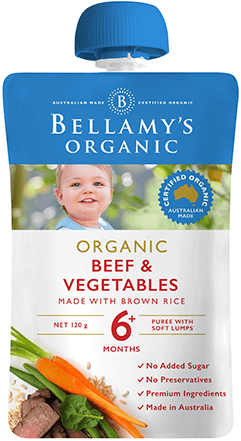 New Packaging
Organic Beef & Vegetables
New Packaging
Organic Beef & Vegetables
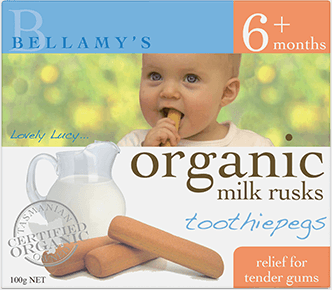 CURRENT Packaging
Organic Milk Rusks Toothiepegs
CURRENT Packaging
Organic Milk Rusks Toothiepegs

 New Packaging
Organic Milk Rusks
New Packaging
Organic Milk Rusks

In babies, signs of coeliac disease may be signalled from gastrointestinal clues such as:
In coeliac disease gluten damages the lining of the small intestine which absorbs the nutrients from our food. Coeliac disease requires life-long avoidance of gluten proteins found in the grains, wheat, spelt, rye, triticale, barley and controversially oats. Once thought of as a childhood disorder that was outgrown, we now know that coeliac disease can be diagnosed at any age. Symptoms of coeliac disease vary a great deal. About twenty percent don’t feel they have any symptoms at diagnosis and about half don’t have gastrointestinal symptoms.
A poor appetite means your baby or child will eat less food. A damaged small intestine means the child will not absorb some of the food it does eat. Therefore other signs to look out for include:
Contrary to this, some children become ravenously hungry when their food nutrients are not being absorbed. If they are eating and drinking lots of food and not gaining weight, this too is a sign to look out for. While some don’t sleep because of discomfort, others sleep more once the fatigue and tiredness sets in.
Coeliac disease shows up after the child starts to eat gluten. In children who carry the genes associated with coeliac disease, gastroenteritis infections early in life, may be one environmental trigger that makes your child more susceptible to developing coeliac disease. If concerned, breast feeding mothers can continue to eat wheat themselves. If the child has coeliac disease, the enzymes to break down lactose (milk sugar) are reduced or lost when the small bowel is damaged by gluten. Going lactose free may help ease symptoms, but this is only masking the real problem.
After you have introduced gluten foods to your child, if you notice any of the changes above and they are unexplained and not resolving, investigate them with your baby’s doctor as soon as possible. Getting a proper medical diagnosis is important. The usual coeliac-specific antibody screen is not so useful in babies under two years and is more accurate in children over five years of age. A small bowel biopsy might be advised. Be guided by your doctor and Paediatric Gastroenterologist. It’s important to see a dietitian who specialises in coeliac disease to help you manage a gluten free diet for your child.
1. Brown AC. Gluten sensitivity: problems of an emerging condition separate from celiac disease. Expert Review of Gastroenterology & Hepatology, 2012;6(1), 43-55, DOI: 10.1586/egh.11.79
2. Myléus et al. Early infections are associated with increased risk for celiac disease: an incident case-referent study. BMC Pediatrics 2012, 12:194 http://www.biomedcentral.com/1471-2431/12/194